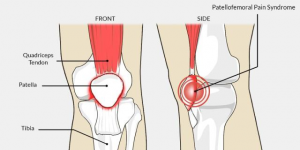
Patellofemoral Pain Syndrome (PFPS) is a common knee complaint that involves pain behind or around the kneecap. It is also known as anterior knee pain.
How common is Patellofemoral Pain?
From 25% to 43% of the active population will have an episode of PFPS in their lifetime. It is the most common condition affecting runners, but is also exacerbated by cycling, squatting, stairs and sitting with a bent knee.
What contributes to PFPS?
The most common risk factors for anterior knee pain include:
- Gender: Women are more at risk than men. Women generally have wider pelvis, which results in a larger ‘Q angle’ at the knee. This changes the way
 load is taken through the knees and can increase susceptibility to PFPS.
load is taken through the knees and can increase susceptibility to PFPS.
- Running: PFPS is the most common condition in runners, especially with large fluctuations with load (increases in running distance or time for example)
- Muscle weakness: Weakness in thigh muscles (quadriceps group) is the most common risk factor for developing PFPS. Weakness in the hip muscles can contribute to poor biomechanics and also is a risk factor for PFPS
- Muscle length: Some studies have shown an association with tightness in quadriceps, hamstrings, IT band and calf muscles
- Biomechanics: Increase in Q angle (mentioned above) can contribute to PFPS. There is also some research to say foot position during walking/physical activity can play a part in exacerbating the knee joint
- Change in activity: Often PFPS occurs after a sudden increase in load, especially big increases in running distance or pace
- Altered muscle activation: Some studies have shown changes in the order of activation of muscles in the quadriceps muscle group, creating a disordered pull of the kneecap during walking, running, squatting etc.

Does this pain ring any bells for you? It might be time to seek physiotherapy opinion.
What can physios do?
ADVICE AND EXPLANATION: Your physio will give you a detailed explanation of the condition and the rehabilitation you will require to return to full function. Includes home exercise program, what activties to avoid while healing, and gradual progression of physical activity.
TAPE: Rigid taping or Kinesio taping, aimed to correct patella position which relieved pain and allows retraining of the knee muscles to occur.
SOFT TISSUE THERAPY: Massage and dry needling are often effective at reducing the tightness and tone in the hip and quad muscles which takes pressure of the knee joint and allows more freedom of movement.
EXERCISE: The most important aspect of recovery is getting stronger and more flexible, especially through the hips, thighs and calf muscles.
BIOMECHANICS: Depending on your individual causes of PFPS, it may be helpful to be fitted with foot orthotics, which can help provide better shock absorption at your feet and better knee alignment in the short-term (12 months).
WHAT DOESN’T HELP: Knee braces and surgery. Neither of these have been found to be helpful in improving pain or function in patients with PFPS
How much physio?
The amount of treatment needed and time taken to recovery differs between case to case, as each individual will have a varied combination of risk factors that need to be addressed and adjusted.
We generally recommend 2-3 treatments per week initially to settle symptoms, followed by less frequent appointments to manage progressions in strength and load, so we can get you back to your strongest and fittest self!
If you’ve got knee pain and would like us to help you with it, simply go to our online booking page where you can find a time that suits you and book yourself in 24/7.

